Zha Lab

Location and Contact Information
Principal Investigator
Cancer is a genetic disease. DNA alterations drive the initiation, progression, metastasis, and relapse of human cancers. Thus, preservation of genome integrity is critical to suppress tumor formation in all cell types. Yet, in lymphoid cells, programmed somatic gene rearrangements are essential for the proper development of an adaptive immune system in which diverse pathogens are specifically recognized and committed to immunological “memory.” As such, developing lymphocytes face the daunting task of maintaining genomic stability while executing multiple rounds of physiological gene rearrangements. Not surprisingly, defects in DNA repair pathways can block lymphocyte development, leading to congenital primary immunodeficiency. Such defects also increase the risk of aberrant DNA rearrangements, including the pathogenic chromosomal translocations that elicit leukemia and lymphoma. Finally, current chemotherapy targets fast growing cancer cells by introducing deliberating DNA damages. Therefore, elucidating the cellular pathways that mediate DNA repair, understanding their molecular mechanisms of action, and evaluating their in vivo functions in animal models will yield critical information for the clinical management of both immunodeficiency and cancer.
Double-strand DNA breaks (DSBs), which entail cleavage of both strands of the double-helix, are the most toxic form of DNA damage. Consequently, mammalian cells rely on multiple distinct pathways of DSB repair, including non-homologous end-joining (NHEJ). DSBs trigger robust DNA damage responses orchestrated primarily by three PI3 kinase-related protein kinases (PI3KKs): ATM, DNA-PK and ATR. When activated, the ATM, DNA-PK, and ATR kinases phosphorylate over 800 overlapping protein substrates to promote efficient and accurate DSB repair and also eliminate cells with persistent DNA damages. While all cell types can acquire DSBs upon exposure to exogenous agents, such as radiation or genotoxic chemotherapy, developing lymphocytes also undergo programmed DSBs during the assembly of the immunoglobulin (Ig) and the T cell receptor (TCR) genes from the germline Variable (V), Diversity (D), and Joining (J) gene segment in a process termed V(D)J recombination. In addition, upon antigen exposure, naïve B lymphocytes experience two additional gene modification events - somatic hypermutation (SHM) and class switch recombination (CSR) to achieve higher affinity and different effector function respectively. While these physiological DSBs were initiated by lymphocyte-specific genes, they trigger robust DNA damage responses and require the NHEJ repair pathway for completion. As such, lymphocyte gene rearrangement has been a powerful system to study the mechanisms by which cells respond and repair DSBs in vivo.
Our research is focused on the fundamental mechanisms by which cells respond to DNA damage, especially DSBs, and how these responses impact normal lymphocyte development, lymphomagenesis, and cancer therapy. In the past eight years, we have made significant progresses on several fronts through the identification of:
- Activity-dependent structural functions of the ATM, ATR DNA-PK kinases in DNA repair (PNAS 2011, JCB 2012, Mol Cell 2015, Elife 2016)
- Several new NHEJ repair factors (XLF/Cernunnos, PAXX and MRI) and their roles in DNA repair and primary immunodeficiency (Mol Cell 2008, Nature 2011, PNAS 2012, Blood 2014, Nature Comm 2017)
- New translocation mechanisms and tumor suppressor genes (e.g. Bcl11b) relevant to human leukemia (JEM 2010, Blood 2011, Blood 2015, JHemaOnc 2015 and Leukemia 2015)
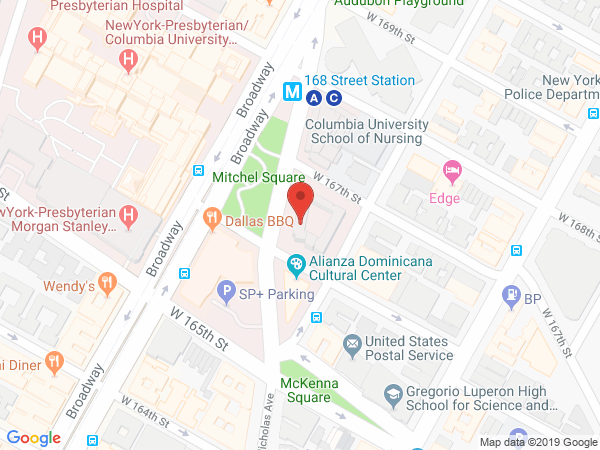
The Zha Lab is located in the Institute For Cancer Genetics (ICG) at Columbia University. Visit Dr. Zha's ICG lab page.